stress urinary incontinence
Stress Urinary Incontinence SUI
1:3 women who ever have a baby will experience some SUI during their life!!
SUI occurs when your pelvic floor muscles are weakened from an outside influence, like a cough, laugh or sneeze, which causes a small amount of urine to leak from the bladder.
Stress incontinence is often treated by pelvic floor exercises.
Urgency UI occurs when you have a sudden urge to empty your bladder and leak urine on the way to the toilet. SUI is most prevalent in women during and after they have had children. During pregnancy the position and weight of the growing baby on top of the bladder can cause frequency (needing to go often) and sometimes urgency (sudden and overwhelming desire to go to the toilet).
Some pregnant women may experience small leaks with a full bladder when they cough, sneeze, laugh, run, jump, etc. and this may continue after the birth of their baby. This is not normal and should be addressed with correct pelvic floor muscle awareness and activation during pregnancy. it’s NOT OK to accept this as ‘normal’ after the birth of your baby as it may lead to long term problems.
” Although commonly seen in middle aged and elderly women when a group of female student nurses who had not had children where questioned, 40% admitted some form of incontinence. Many women avoid seeking medical help due to the misconception that the condition is a normal part of ageing or due to embarrassment.”
Types of SUI
| Stress | Involuntary leakage on effort or exertion, or on sneezing or coughing |
| Urge | Involuntary leakage accompanied by or immediately preceded by urgency |
| Mixed | Involuntary leakage associated with urgency and also with exertion, effort, sneezing, or coughing |
| Functional | Untimely urination because of physical disability, external obstacles, or problems in thinking or communicating that prevent a person from reaching a toilet |
| Overflow | Unexpected leakage of small amounts of urine because of an overfilled bladder |
| Transient | Leakage that occurs temporarily because of a condition or situation that will pass (eg, infection, medication) |
| Deformity | Fistula or developmental abnormality |
On the pelvic floor page I directed you to several websites to explain where and how the pelvic floor muscles work.
Let’s just have a quick anatomy review.
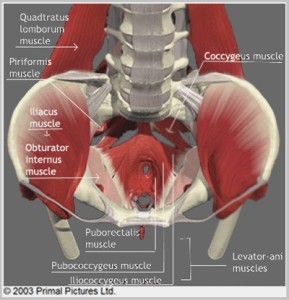
The pelvic floor muscles are on the inside of your pelvis. They sling between the pubic bone at the front and the tailbone at the back. They also run across the back of the pelvis inside between the two bones that you sit on. They are there to keep the bladder, bowel, and uterus up in the pelvis and control the emptying of bladder and bowel. The pelvic floor muscles also play a role in sexual satisfaction and orgasm.
This picture on the right shows a view down into the bowl of the pelvis. You can see the Pubococcygeus, Puborectalis, and Coccygeus muscles. These form the ‘Levator Ani’ muscles. This ‘plate’ of muscles, fascia and ligaments keep the bladder, uterus and bowel up inside the pelvis and controls the emptying of bladder and bowel.
These techniques can assist women find their pelvic floor muscles:
•When emptying the bladder try to stop or slow the stream. Do this only to help identify the pelvic floor and not as a regular exercise. Do not perform this technique if you suffer from bladder emptying problems.
•Imagine you are trying to avoid passing wind in doing so attempt to lift and squeeze the muscles in and around the anus. Your buttocks should stay relaxed and your breathing should remain regular.
•Use a mirror to view the entrance to your vagina. Try to lift and squeeze in and around the entrance of your vagina. You should see a squeeze and inwards lift of the vaginal entrance.
There are also good videos on you tube explaining the anatomy of this area.
Symptoms of stress urinary incontinence SUI
•accidentally leaking urine when you exercise, laugh, cough or sneeze
•needing to get to the toilet in a hurry or not making it there in time
•constantly needing to go to the toilet
•accidentally losing control of your bladder or bowel
•accidentally passing wind
These symptoms are the result of the muscles around the bladder neck or sphincter not being able to contract enough to withstand the pressures from the pelvic and abdominal cavity above.
Women’s health physiotherapists describe this as the ‘intra- abdominal pressure’ IAP exceeding the ‘intra vaginal pressure’ and therefore causing ‘stress’ leaks.
Some women only experience this with a full bladder and think that it’s OK …it’s still stress urinary incontinence…and we must NOT be soothed by our various incontinence product manufacturers to believe that ‘light bladder leakage’ is the norm.
I feel so much better now I have got that off my chest!
So what to do now….
If you are not confident that you can identify and contract the pelvic floor muscles
- contact me for an assessment
- see your GP if you are concerned to exclude other pathology
- reduce your ‘stresses’ on your pelvic floor
- reduce lifting small and large children
- address excess weight with a ‘safe’ exercise programme
- reduce any coughing or sneezing due to viruses, chronic chest problems or allergies by reviewing your medications
- if you are doing high impact exercises- running , bootcamp / boy exercises and ignoring the problem STOP now you are only making the problem worse
- if you work with a personal trainer, tell them your problem- you would do so if you had a sore knee or back injury. If they can’t modify your programme …come and see me. I love putting my personal trainer hat on and guiding you into safe exercise options
Sometimes pelvic floor exercises are not enough and don’t fix the problem. We, as women’s health physios need to be able to admit this and refer on to GP – Urogynae – Gynae – Colo rectal specialists for further advice / investigation and possible surgery.
So what are the surgical options for SUI
Surgery is only recommended after the exact cause of urinary incontinence has been found. Strengthening exercises are still the 1st treatment approach generally for SUI
Colposuspension – this procedure involves the bladder neck being lifted back to its proper position. The front wall of the vagina (where the urethra is located) is lifted and stitched to strong ligaments near the pubic bone. The most popular type of colposuspension procedure is Burch colposuspension, which can be performed both abdominally and laparoscopically (key-hole surgery).
Sling procedure – in this procedure, a piece of fascia (strong tissue that covers the body’s muscles) or a synthetic material such as mesh tape, is placed under the urethra like a hammock to support it. Some sling procedures are performed while you are under a general anaesthetic, while others can be done using a regional anaesthetic. The procedure generally requires small incisions in the abdomen and/or vagina.
Surgery should only be considered after you have trialled conservative treatments and undergone a urodynamic assessment to ensure the diagnosis is correct and your condition is favourable to surgical correction. Success rates and risks vary for different procedures and so you should discuss this with your doctor prior to surgery. Surgery may not result in a complete resolution of incontinence symptoms. Surgery is generally not performed unless a woman is not planning any further pregnancies, as pregnancy will impact the ongoing results.
Intrinsic Sphincter Deficiency ISD
ISD another type of SUI where the urethra (tube from your bladder) lacks the normal closing pressure needed to prevent leakage on activities. In ISD, the bladder outlet is open at rest and urine can leak through even with lighter impact activities. It’s like a garden hose that you stand on…but not quite enough to stop the flow .
The neck of the bladder is not staying closed ‘tightly’ The most severe form of ISD-related stress urinary incontinence is that of the fixed ‘lead-pipe’ urethra.
Closure is achieved by a combination of factors including the strength of the connective tissue, (intact pelvic fascia and ligaments) the blood flow to the urethra, the health of the lining of the urethra and the strength of the muscle surrounding the urethra.
Several problems may compromise this closure:
- Tearing of the nerves to the sphincter during childbirth
- Peripheral neuropathies as occur with diabetes and other causes.
- Increased age.
- The lack of Oestrogen in that area in the post-menopausal phase of a woman’s life.
- Trauma from surgery [e.g. vaginal repair, urethrotomy].
Intrinsic Sphincter Deficiency [ISD] is diagnosed by Urodynamic Studies measuring the Urethral closure pressure UCP. This involves a catheter being inserted into your urethra . Sydney Urodynamics is staffed by experienced Urogynaecologists
There are several other indicators in the client history and symptoms which will help the Women’s health physiotherapist with this diagnosis.
Prevention – maintenance of good pelvic floor muscles
Treatment:
1. Local oestrogen in vaginal cream or pessary long term.
2. Alpha adrenergic agonists—these drugs may stimulate the sphincter.
3. Injection of peri-urethral bulking agents e.g. Macroplastique.
Success, however is limited making prevention even more important.
The absolute 1st line of action or “best practise” medicine is to try and strengthen your Pelvic floor muscles. Most GP’s, Gynaecologists and Urogynaecologist’s will advise their patients to try 3-6months of Pelvic floor muscle education and re- training before surgical intervention.